Step 2 of 8
Neonatal physiology
The clinical evolution of most congenital heart defects is improved if the defects are corrected at a young age. This raises issues for anaesthetists who treat children aged under one year, whose heart, organs and haemodynamic regulation are not yet fully developed.
Special features of the neonatal heart
At birth, both ventricles are the same size and the same thickness, but the LV must very quickly accommodate an increase of its afterload, whereas the RV faces a decline in its afterload since the PAP reaches its normal value after the end of the 2nd month of life. The LV is hypertrophic, and its mass is approximately double that of the RV after 6 months [8].
A newborn’s heart is immature. It contains less contractile fibres than that of an adult (30% versus 60%); these fibers are not yet well organised. The heart develops less tension per unit of mass than that of an adult. Sympathetic innervation is incomplete, and catecholamine reserves are low. The density of β1 receptors is poor, α1 receptors predominate; in cyanotic children, the concentration of β2 receptors is also decreased [10]. In the case of important stress, myocardial contractility and peripheral vascular tone therefore depend largely on an exogenous contribution of catecholamines by the adrenal glands. The decrease in β-receptors explains the better efficacy of adrenaline (α1 effect) and of milrinone (independent of β receptors pathway) compared to dopamine or dobutamine. By contrast, parasympathetic innervation is normal, hence the vagal response prevails in a newborn. The immaturity of the sarcoplasmic reticulum system as a source of free Ca2+ for myocardial contraction makes a small child depend on the membrane transport of Ca2+ to activate tropomyosin; it therefore develops a lower contractile force and slowed relaxation, and depends more on an external contribution of Ca2+ in the case of haemodynamic stress [2]. Infant myocardium is therefore very sensitive to interference with the calcium metabolism. Due to this fact, calcium channel blockers are contraindicated during the first year of life, and cardioplegia solutions are preferentially hypercalcemic [1]. A newborn’s heart depends largely on glycolysis and lactate, but very little on the oxidation of fatty acids, as a source of energy. This relative ability to operate by anaerobic glycolysis makes it more resistant to ischaemia.
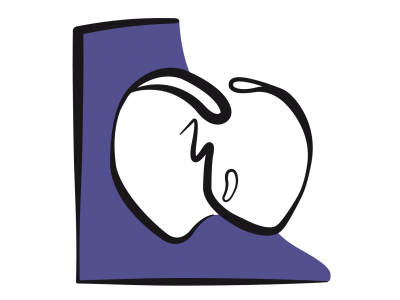
The compliance of heart cavities is low during the first few months of life and the similarity of the ventricles at birth accentuates their interdependence. Thus, a failure of one of the ventricles accompanied by an increase in its end-diastolic pressure (EDP) causes a displacement of the septum which restricts the filling of the other cavity: the failure of a ventricle quickly leads to biventricular congestive failure. The reduced compliance of the ventricles makes them extremely sensitive to preload variations: small increases in volume rapidly lead to a high elevation of filling pressure. The shape of the Frank-Starling curve is different from that of an adult: the slope of the ascending part is very steep, which means that systolic volume is strongly dependent on the preload. But the curve reaches its plateau very quickly (around 5-8 mm Hg), from which point an increase in preload is no longer translated by an increase in systolic volume but only by an elevation of filling pressure (Figure 14.7) [2,11].
Special features of the neonatal heart
At birth, both ventricles are the same size and the same thickness, but the LV must very quickly accommodate an increase of its afterload, whereas the RV faces a decline in its afterload since the PAP reaches its normal value after the end of the 2nd month of life. The LV is hypertrophic, and its mass is approximately double that of the RV after 6 months [8].
A newborn’s heart is immature. It contains less contractile fibres than that of an adult (30% versus 60%); these fibers are not yet well organised. The heart develops less tension per unit of mass than that of an adult. Sympathetic innervation is incomplete, and catecholamine reserves are low. The density of β1 receptors is poor, α1 receptors predominate; in cyanotic children, the concentration of β2 receptors is also decreased [10]. In the case of important stress, myocardial contractility and peripheral vascular tone therefore depend largely on an exogenous contribution of catecholamines by the adrenal glands. The decrease in β-receptors explains the better efficacy of adrenaline (α1 effect) and of milrinone (independent of β receptors pathway) compared to dopamine or dobutamine. By contrast, parasympathetic innervation is normal, hence the vagal response prevails in a newborn. The immaturity of the sarcoplasmic reticulum system as a source of free Ca2+ for myocardial contraction makes a small child depend on the membrane transport of Ca2+ to activate tropomyosin; it therefore develops a lower contractile force and slowed relaxation, and depends more on an external contribution of Ca2+ in the case of haemodynamic stress [2]. Infant myocardium is therefore very sensitive to interference with the calcium metabolism. Due to this fact, calcium channel blockers are contraindicated during the first year of life, and cardioplegia solutions are preferentially hypercalcemic [1]. A newborn’s heart depends largely on glycolysis and lactate, but very little on the oxidation of fatty acids, as a source of energy. This relative ability to operate by anaerobic glycolysis makes it more resistant to ischaemia.
The compliance of heart cavities is low during the first few months of life and the similarity of the ventricles at birth accentuates their interdependence. Thus, a failure of one of the ventricles accompanied by an increase in its end-diastolic pressure (EDP) causes a displacement of the septum which restricts the filling of the other cavity: the failure of a ventricle quickly leads to biventricular congestive failure. The reduced compliance of the ventricles makes them extremely sensitive to preload variations: small increases in volume rapidly lead to a high elevation of filling pressure. The shape of the Frank-Starling curve is different from that of an adult: the slope of the ascending part is very steep, which means that systolic volume is strongly dependent on the preload. But the curve reaches its plateau very quickly (around 5-8 mm Hg), from which point an increase in preload is no longer translated by an increase in systolic volume but only by an elevation of filling pressure (Figure 14.7) [2,11].
Figure 14.7: Frank-Starling curve of a newborn (in blue) compared to that of an adult (in yellow). At normal filling, the ventricle is at the plateau of the curve; filling variations (EDP, end-diastolic pressure in mmHg) do not alter the stroke volume (SV, in mL/kg) [11].
The flow can continue to increase with the increase in the preload only if the afterload declines. Afterload increases is very poorly tolerated; it causes an early flattening of the Starling curve, whose effect is similar to that of a negative inotropic agent. Cardiac output essentially depends on heart rate, because the stroke volume is relatively fixed and a neonatal heart operates at 95% of its maximum performance.
Organs and systems
The lungs only reach full maturity around the age of 8 years. During childhood, they are very sensitive to the systemic inflammatory response (SIRS) and ischemia-reperfusion lesions, all two characteristics of the CPB. Compared to those of an adult, they are more prone to an interstitial fluid leak (capillary leak syndrome) linked to haemodilution and pulmonary flow variations. The exacerbation of pulmonary hypertension is common in the young who suffer from excessive pulmonary flow (L-to-R shunt, truncus arteriosus, etc.) [5].
The kidneys develop normal excretory capabilities only after the age of 2 years. Until that age, the concentration and dilution mechanisms are not fully functional. With CPB, there is therefore a tendency for greater fluid accumulation in infants than among children aged 2-3 years and above. Postoperative kidney failure is also more common after CPB: 31%, 14% and 7% of children aged under one year develop a stage 1, 2, and 3 acute kidney injury respectively [3]. If the fluid balance is close to zero at the end of the operation, this avoids overloading hypofunctioning kidneys. This is achieved by conventional ultrafiltration during CPB and modified ultrafiltration at the end of the operation [12]. Diuretics (furosemide 1-2 mg/kg, ethacrynic acid 1 mg/kg) are used postoperatively [9]. Coagulation cascade does not fully develop before the age of one year. Hepatic synthesis of vitamin K-dependent clotting factors is lower and coagulation anomalies are common (prolonged PT and aPTT, low concentrations of von Willebrand factor, fibrinogen, and clotting factors V and VIII). Moreover, CPB reduces concentrations of these factors and of platelets by 50-70% [7].
Glycaemic control is poor and the risk of hypoglycaemia is ever-present due to decreased glycogen reserves and hepatic synthesis. Neurological sequelae in infants are linked to the permanent risk of hypoglycaemia rather than to hyperglycaemia [4]. Adult-specific diets aimed at rigorously maintaining normoglycaemia are not appropriate for young children [6].
The kidneys develop normal excretory capabilities only after the age of 2 years. Until that age, the concentration and dilution mechanisms are not fully functional. With CPB, there is therefore a tendency for greater fluid accumulation in infants than among children aged 2-3 years and above. Postoperative kidney failure is also more common after CPB: 31%, 14% and 7% of children aged under one year develop a stage 1, 2, and 3 acute kidney injury respectively [3]. If the fluid balance is close to zero at the end of the operation, this avoids overloading hypofunctioning kidneys. This is achieved by conventional ultrafiltration during CPB and modified ultrafiltration at the end of the operation [12]. Diuretics (furosemide 1-2 mg/kg, ethacrynic acid 1 mg/kg) are used postoperatively [9]. Coagulation cascade does not fully develop before the age of one year. Hepatic synthesis of vitamin K-dependent clotting factors is lower and coagulation anomalies are common (prolonged PT and aPTT, low concentrations of von Willebrand factor, fibrinogen, and clotting factors V and VIII). Moreover, CPB reduces concentrations of these factors and of platelets by 50-70% [7].
Glycaemic control is poor and the risk of hypoglycaemia is ever-present due to decreased glycogen reserves and hepatic synthesis. Neurological sequelae in infants are linked to the permanent risk of hypoglycaemia rather than to hyperglycaemia [4]. Adult-specific diets aimed at rigorously maintaining normoglycaemia are not appropriate for young children [6].
| Infant physiology |
|
Infants’ hearts exhibit low compliance, performance, and functional reserves, and cannot withstand volume or pressure overloads. Cardiac output can only be varied by adjustments in heart rate.
There is a higher risk of hypoglycaemia than hyperglycaemia. The lungs, kidneys, and liver only reach functional maturity from the age of two years. Coagulation underperforms during infants’ first year. |
© BETTEX D, BOEGLI Y, CHASSOT PG, June 2008, last update February 2020
References
- ALLEN BS, BARTH MJ, ILBAWI MN. Pediatric myocardial protection: an overview. Semin Thorac Cardiovasc Surg 2001; 13:56-72
- ANDERSON PAW. Immature myocardium. In: MOLLER JH, NEAL WA (eds). Fetal and Infant cardiac disease. Norwalk, CT:Appleton & Lange, 1990, 35-71.
- BLINDER JJ, GOLDSTEIN SL, LEE VV; et al. Congenital heart surgery in infants: effects of acute kidney injury on outcomes. J Thorac Cardiovasc Surg 2012; 143:368-74
- DE FERRANTI S, GAUVREAU K, HICKEY PR, et al. Intraoperative hyperglycemia during infant cardiac surgery is not associated with adverse neurodevelopmental outcomes at 1, 4, and 8 years. Anesthesiology 2004; 100:1345-52
- DÖNMEZ A, YURDAKÖK O. Cardiopulmonary bypass in infants. J Cardiothorac Vasc Anesth 2014; 28:778-88
- HIRSCH JC, JACOBS ML, ANDROPOULOS D, et al. Protecting the infant brain during cardiac surgery: a systematic review. Ann Thorac Surg 2012; 94:1365-73
- KERN FH, MORANA NJ, SEARS JJ, et al. Coagulation defects in neonates during cardiopulmonary bypass. Ann Thorac Surg 1992; 54:541-6
- LAKE CL. Neonatal myocardial and circulatory function. In: LAKE CL. Pediatric Cardiac Anesthesia, 2nd edition, Norwalk : Appleton & Lange, 1993, 33-42
- PICCA S, RICCI Z, PICARDO S. Acute kidney injury in infant after cardiopulmonary bypass. Semin Nephrol 2008; 28:470-6
- SUN LS, DU F, QUAGEBEUR JM. Right ventricular infundibular -adrenoreceptor complex in tetralogy of Fallot patients. Pediatr Res 1997; 42:12-6
- THORNBURG KL, MORTON MJ. Filling and arterial pressures as determinants of RV stroke volume in the sheep fetus. Am J Physiol 1983,;144:H656-H663.
- WANG S, PALANZO D, ÜNDAR A. Current ultrafiltration techniques before, during and after pediatric cardiopulmonary bypass procedures. Perfusion 2012; 27:438-46
14. Anesthesia for paediatric heart surgery
- 14.1 Introduction
- 14.2 Pathophysiology
- 14.3 Haemodynamic strategies
- 14.3.1 Classification
- 14.3.2 Left-to-right shunt and high pulmonary blood flow
- 14.3.3 Pulmonary hypertension in children
- 14.3.4 Cyanotic right → left shunt and reduced pulmonary blood flow
- 14.3.5 Cyanotic right → left shunt and reduced systemic blood flow
- 14.3.6 Bidirectional cyanotic shunt
- 14.3.7 Heart diseases without shunting: obstructions and valvular heart diseases
- 14.3.8 Treatment options for neonates
- 14.3.9 Drug therapy
- 14.4 Anaesthetic technique
- 14.5 CPB in children
- 14.6 Anaesthesia for specific pathologies
- 14.6.1 Introduction
- 14.6.2 Anatomical landmarks
- 14.6.3 Anomalous venous returns
- 14.6.4 Atrial septal defects (ASDs)
- 14.6.5 Atrioventricular canal (AVC) defects
- 14.6.6 Ebstein anomaly
- 14.6.7 Anomalies of the atrioventricular valves
- 14.6.8 Ventricular septal defects (VSDs)
- 14.6.9 Ventricular hypoplasia
- 14.6.10 Tetralogy of Fallot
- 14.6.11 Double outlet right ventricle (DORV)
- 14.6.12 Pulmonary atresia
- 14.6.13 Anomalies of the left ventricular outflow
- 14.6.14 Transposition of the great arteries (TGA)
- 14.6.15 Truncus arteriosus
- 14.6.16 Coarctation of the aorta
- 14.6.17 Arterial abnormalities
- 14.6.18 Heart transplantation
- 14.7 Conclusions