Step 15 of 18
Truncus arteriosus
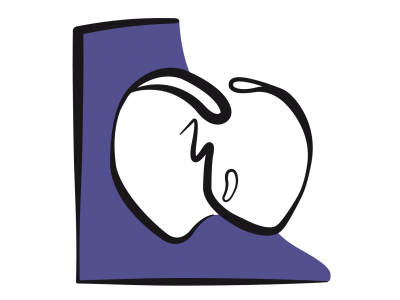
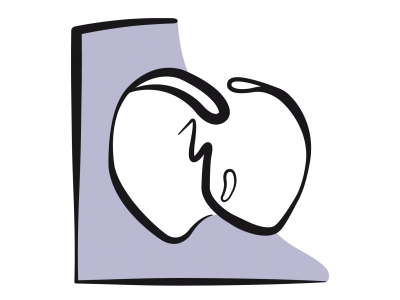
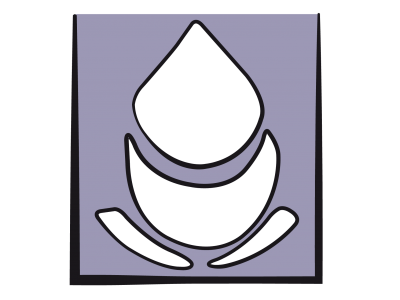
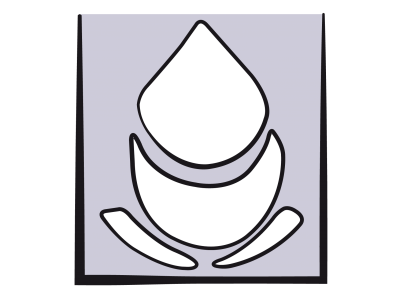
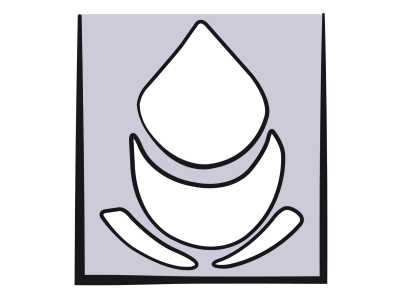
In truncus arteriosus, the aorta and pulmonary artery originate from a common vessel overriding a VSD. This vessel has a single large 3-4 leaflet ventriculoarterial valve, which is often dysplastic and insufficient, and sometimes stenosing. There are four types of truncus (Figure 14.70) [3].
- Type 1: the PA is rooted on the left lateral side of the common vessel;
- Type 2: both pulmonary arteries originate separately from the truncus;
- Type 3: only one pulmonary artery is present and the contralateral lung is vascularised by collaterals or bronchial arteries (MAPCA: major aortopulmonary collateral arteries);
- Type 4: defined by the presence of an interrupted aortic arch rather than the origin of the PA, since the origin of the PAs is variable.
Figure 14.70: Diagram of the various types of truncus arteriosus. A: type 1 – the PA is rooted on the left lateral side of the common vessel. B: type 2 – both pulmonary arteries originate separately from the truncus. C: type 3 – only one pulmonary artery is present and the other is replaced by a large collateral artery or bronchial arteries (Coll). D: type 4 – the aortic arch is interrupted (IAA) after the brachiocephalic trunk, and the aortic arch and descending aorta (Ao) follow on from the ductus arteriosus (DA). The origin of the PAs is variable [3].
A wide VSD equalises the systemic and pulmonary pressure and prompts a complete mixture of venous and arterialised blood, resulting in hypoxaemia and cyanosis. The Qp:Qs ratio is dependent on the ratio between PVR and SVR (single ventricle physiology). As the PVR falls after birth, pulmonary flow increases at the expense of systemic flow, resulting in metabolic acidosis. To restore the balance, PVR must be increased (hypoxia, hypercapnia). If ventriculoarterial valve insufficiency is present, the ventricles are also subjected to volume overload.
The malformation is associated with DiGeorge syndrome in 20-25% of cases. This syndrome is characterised by intubation difficulties, a risk of hypocalcaemia, and a high risk of infection. The heart disease rapidly becomes symptomatic after birth, with the appearance of moderate cyanosis and congestive ventricular insufficiency. Diastolic pressure is low due to leakage into the pulmonary vascular bed, entailing a risk of subendocardial ischaemia. The pulmonary circulation is overloaded and subjected to systemic pressure. Unless the flow is restricted (banding), irreversible pulmonary hypertensive vascular lesions develop quickly.
Surgical correction is performed within 10 to 20 days of birth [2]. It involves a patch over the VSD, which redirects the LV flow to the aorta (in this case, the truncus). The neoaortic valve is rebuilt or replaced if it is insufficient. The PA is disconnected from the trunk and anastomosed to a RV-PA valved conduit (homograft, Contegra™). In some cases, a small relief ASD is created if right-side pressure is very high. While this helps to maintain cardiac output, it also causes arterial desaturation. The surgical mortality rate is 5-18% [1]. Aggravating factors are: young age (< 1 month), valvular insufficiency, ventricular failure, and the presence of coronary artery anomalies or interrupted aortic arch.
An aortopulmonary window is a wide congenital fistula between the ascending aorta and the trunk of the PA. Although not anatomically related to truncus arteriosus, it functions in the same way from a haemodynamic perspective and involves the same anaesthetic constraints.
Anaesthesia
The aim is to maintain adequate systemic flow while minimising pulmonary flow to achieve balanced Qp/Qs (Qp/Qs = 1). The initiation of CPB is sometimes precipitated by refractory Qp/Qs imbalance.
- Hypoventilation, hypercapnia (potentially FiCO2 2-4%), FiO2 0.21-0.3.
- PEEP 5-10 cm H2O.
- Systemic vasodilation: arterial pressure must nevertheless remain sufficient to ensure coronary perfusion, especially if ventriculoarterial valve insufficiency lowers arterial diastolic pressure.
- Inotropic support: milrinone (0.5-1.0 mcg/kg/min) ± epinephrin (0.01-0.1 mcg/kg/min).
- Deep anaesthesia with high doses of fentanyl (50-100 mcg/kg), adjunction of midazolam, and potentially etomidate for induction.
By tightly banding the PA on opening the pericardium, it is possible to temporarily control pulmonary flow for the initiation of CPB. Post-CPB, it is important to prevent pulmonary hypertensive crises (hyperventilation, fentanyl, NO•, PGE1, magnesium, normothermia) as these children have a hyperreactive pulmonary vascular tree and PAH is common. Insertion of a catheter in the PA is recommended for continuous measurement of SvO2. Inotropic support (dobutamine, epinephrin-milrinone) is usually required. Patients are extubated late (> 24 hours).
The most common immediate complications are PAH crises with RV failure, LV failure, neoaortic valve regurgitation, and complete AV block. In the long term, the repair and conduit become relatively stenotic as the child grows and reoperation is necessary.
The most common immediate complications are PAH crises with RV failure, LV failure, neoaortic valve regurgitation, and complete AV block. In the long term, the repair and conduit become relatively stenotic as the child grows and reoperation is necessary.
| Truncus arteriosus |
|
The aorta and pulmonary artery originate from a common vessel overriding a VSD. Management: increase systemic flow and reduce pulmonary flow to achieve Qp/Qs = 1
- Hypoventilation, hypercapnia, respiratory acidosis, systemic vasodilation - Risk of ischaemia if low diastolic pressure (ventriculoarterial valve insufficiency) - Congestive ventricular failure (dobutamine, milrinone) After correction, high risk of pulmonary arterial hypertension and congestive ventricular failure |
© BETTEX D, BOEGLI Y, CHASSOT PG, June 2008, last update May 2018
References
- BROWN JW, RUZMETOV M, OKADA Y, et al. Truncus arteriosus repair : outcomes, risk factors, reoperation and managment. Eur J Cardiothorac Surg 2001 ; 20 :221-7
- HONJO O, Van ARSDELL GS. Cardiovascular procedures : surgical considerations. In : BISSONNETTE B, edit. Pediatric anesthesia. Basic principles, State of the art, Future. Shelton (CO): People’s Medical Publishing House (USA), 2011, 1589-608
- VAN PRAAGH R, VAN PRAAGH S. The anatomy of common aortico-pulmonary trunk (truncus arteriosus communis) and its embryologic implications. A study of 57 necropsy cases. Am J Cardiol 1965; 16:406-25
14. Anesthesia for paediatric heart surgery
- 14.1 Introduction
- 14.2 Pathophysiology
- 14.3 Haemodynamic strategies
- 14.3.1 Classification
- 14.3.2 Left-to-right shunt and high pulmonary blood flow
- 14.3.3 Pulmonary hypertension in children
- 14.3.4 Cyanotic right → left shunt and reduced pulmonary blood flow
- 14.3.5 Cyanotic right → left shunt and reduced systemic blood flow
- 14.3.6 Bidirectional cyanotic shunt
- 14.3.7 Heart diseases without shunting: obstructions and valvular heart diseases
- 14.3.8 Treatment options for neonates
- 14.3.9 Drug therapy
- 14.4 Anaesthetic technique
- 14.5 CPB in children
- 14.6 Anaesthesia for specific pathologies
- 14.6.1 Introduction
- 14.6.2 Anatomical landmarks
- 14.6.3 Anomalous venous returns
- 14.6.4 Atrial septal defects (ASDs)
- 14.6.5 Atrioventricular canal (AVC) defects
- 14.6.6 Ebstein anomaly
- 14.6.7 Anomalies of the atrioventricular valves
- 14.6.8 Ventricular septal defects (VSDs)
- 14.6.9 Ventricular hypoplasia
- 14.6.10 Tetralogy of Fallot
- 14.6.11 Double outlet right ventricle (DORV)
- 14.6.12 Pulmonary atresia
- 14.6.13 Anomalies of the left ventricular outflow
- 14.6.14 Transposition of the great arteries (TGA)
- 14.6.15 Truncus arteriosus
- 14.6.16 Coarctation of the aorta
- 14.6.17 Arterial abnormalities
- 14.6.18 Heart transplantation
- 14.7 Conclusions