Step 6 of 9
Bidirectional cyanotic shunt
In these pathologies (total anomalous pulmonary venous return, wide VSD, single AV valve, single ventricle, TGA, truncus arteriosus), the pulmonary system is not protected by stenosis (Figure 14.17 and Figure 14.21).

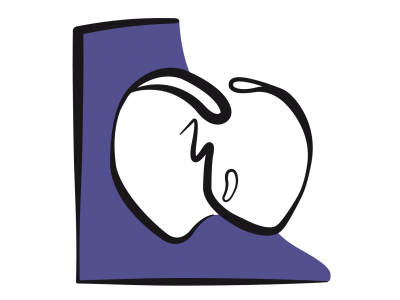
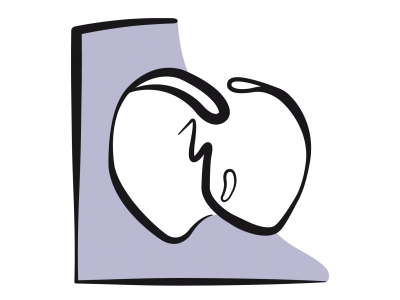
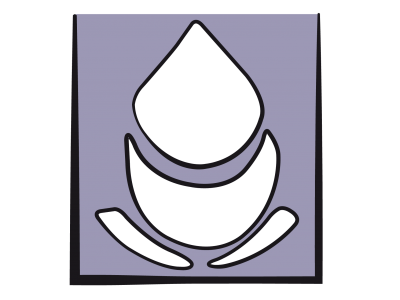
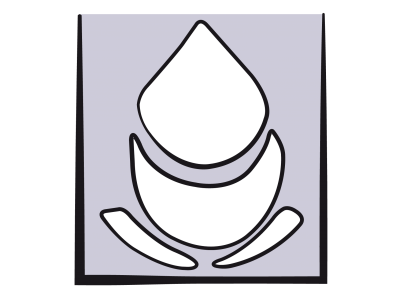
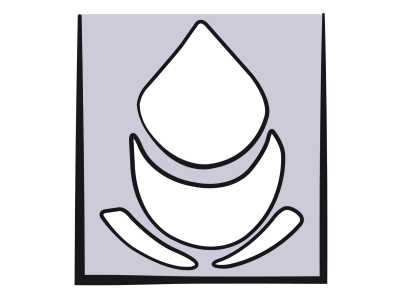
Figure 14.21: Diagram of a cyanotic R-to-L shunt involving a mixture of venous and arterial blood in a double-outlet single ventricle (SV). The image shows a case of hypoplastic right heart syndrome with tricuspid atresia (green arrow). The SV is of left ventricular anatomical type. Blood flows from the RV to the LV through a VSD (blue arrow). The pulmonary artery (PA) and aorta (Ao) stem from the same ventricle. Blood flows between the right and left-side circulation through a wide atrial septal defect (ASD).
Distribution of blood flow between the aorta and PA is directly dependent on the balance between systemic and pulmonary arterial resistance. Anatomical variations determine whether the highest level of blood flow is sent to the pulmonary or systemic vascular tree [2].
In heart diseases where arterialised blood mixes with venous blood, the degree of cyanosis (SaO2 ≤ 85%) is dependent on the ratio between the pulmonary blood flow (Qp) and systemic blood flow (Qs). Since cyanotic children adapt to low SaO2, the aim is to achieve a Qp/Qs ratio close to 1:1 rather than the highest possible SaO2. This often equates to SaO2 of 75-85%. Seeking optimal SaO2 would risk excessive pulmonary blood flow. This would result in ventricular decompensation and low systemic blood flow combined with ischaemia and metabolic acidosis [2].
Choices in terms of haemodynamic management are determined by whether the systemic or pulmonary blood flow is predominant. Children with pulmonary overload are particularly difficult to stabilise: hyperventilation and hyperoxaemia further increase pulmonary blood flow and cause ventricular decompensation, while hypoventilation and low FiO2 increase the shunt and cyanosis.
Figure 14.21: Diagram of a cyanotic R-to-L shunt involving a mixture of venous and arterial blood in a double-outlet single ventricle (SV). The image shows a case of hypoplastic right heart syndrome with tricuspid atresia (green arrow). The SV is of left ventricular anatomical type. Blood flows from the RV to the LV through a VSD (blue arrow). The pulmonary artery (PA) and aorta (Ao) stem from the same ventricle. Blood flows between the right and left-side circulation through a wide atrial septal defect (ASD).
Distribution of blood flow between the aorta and PA is directly dependent on the balance between systemic and pulmonary arterial resistance. Anatomical variations determine whether the highest level of blood flow is sent to the pulmonary or systemic vascular tree [2].
In heart diseases where arterialised blood mixes with venous blood, the degree of cyanosis (SaO2 ≤ 85%) is dependent on the ratio between the pulmonary blood flow (Qp) and systemic blood flow (Qs). Since cyanotic children adapt to low SaO2, the aim is to achieve a Qp/Qs ratio close to 1:1 rather than the highest possible SaO2. This often equates to SaO2 of 75-85%. Seeking optimal SaO2 would risk excessive pulmonary blood flow. This would result in ventricular decompensation and low systemic blood flow combined with ischaemia and metabolic acidosis [2].
Choices in terms of haemodynamic management are determined by whether the systemic or pulmonary blood flow is predominant. Children with pulmonary overload are particularly difficult to stabilise: hyperventilation and hyperoxaemia further increase pulmonary blood flow and cause ventricular decompensation, while hypoventilation and low FiO2 increase the shunt and cyanosis.
| Bidirectional cyanotic shunt |
|
Mixture of arterial and venous blood, excessive pulmonary blood flow
Aim for Qp/Qs close to 1:1, even if SaO2 remains low |
© BETTEX D, BOEGLI Y, CHASSOT PG, Juin 2008, June 2008, last update May 2018
References
- BENT ST. Anesthesia for left-to-right shunt lesions. In : ANDROPOULOS DA, et al, eds. Anesthesia for congenital heart disease. Oxford: Blackwell-Futura, 2005, 297-327
- BROWN JW, RUZMETOV M, OKADA Y, et al. Truncus arteriosus repair : outcomes, risk factors, reoperation and managment. Eur J Cardiothorac Surg 2001 ; 20 :221-7
14. Anesthesia for paediatric heart surgery
- 14.1 Introduction
- 14.2 Pathophysiology
- 14.3 Haemodynamic strategies
- 14.3.1 Classification
- 14.3.2 Left-to-right shunt and high pulmonary blood flow
- 14.3.3 Pulmonary hypertension in children
- 14.3.4 Cyanotic right → left shunt and reduced pulmonary blood flow
- 14.3.5 Cyanotic right → left shunt and reduced systemic blood flow
- 14.3.6 Bidirectional cyanotic shunt
- 14.3.7 Heart diseases without shunting: obstructions and valvular heart diseases
- 14.3.8 Treatment options for neonates
- 14.3.9 Drug therapy
- 14.4 Anaesthetic technique
- 14.5 CPB in children
- 14.6 Anaesthesia for specific pathologies
- 14.6.1 Introduction
- 14.6.2 Anatomical landmarks
- 14.6.3 Anomalous venous returns
- 14.6.4 Atrial septal defects (ASDs)
- 14.6.5 Atrioventricular canal (AVC) defects
- 14.6.6 Ebstein anomaly
- 14.6.7 Anomalies of the atrioventricular valves
- 14.6.8 Ventricular septal defects (VSDs)
- 14.6.9 Ventricular hypoplasia
- 14.6.10 Tetralogy of Fallot
- 14.6.11 Double outlet right ventricle (DORV)
- 14.6.12 Pulmonary atresia
- 14.6.13 Anomalies of the left ventricular outflow
- 14.6.14 Transposition of the great arteries (TGA)
- 14.6.15 Truncus arteriosus
- 14.6.16 Coarctation of the aorta
- 14.6.17 Arterial abnormalities
- 14.6.18 Heart transplantation
- 14.7 Conclusions