Step 2 of 5
Shunts
Communications (shunts) may occur in the atrial septum (ASDs), interventricular septum (VSDs) or the crux of the heart (AV canal defects). Shunts may also appear in the central veins (abnormal pulmonary venous connections) or great arteries (patent ductus arteriosus, aortopulmonary or coronary fistula). Shunts are defined in terms of the ratio of pulmonary blood flow (Qp) to systemic blood flow (Qs). In normal haemodynamics, the two flows are equal: Qp = Qs. In L-to-R shunts, the Qp/Qs ratio is > 1. If this reaches > 1.5-2, surgery is indicated, as the pulmonary blood flow is twice the systemic blood flow. In R-to-L shunts, the Qp/Qs ratio is < 1. A ratio of 0.5:1 indicates that the pulmonary blood flow is half the systemic blood flow. Therapy is indicated for all R-to-L shunts. Shunts exhibit four main characteristics [5].
- Flow direction. This may be right → left (R-to-L), left → right (L-to-R), or bidirectional. R-to-L shunts are cyanotic. A shunt’s flow is systolic and diastolic with two peaks in velocity – maximum velocity is normally 1 to 4 m/s [1]. Independently from its dimensions, the flow of a shunt increases if the upstream pressure rises or the downstream pressure drops. In the event of systemic arterial vasodilation, the flow of a L-to-R shunt (non-cyanotic) decreases, while that of a R-to-L shunt (cyanotic) increases. To reduce a cyanotic shunt, pulmonary resistance and right-sided afterload must be lowered or systemic resistance and left-sided afterload increased (see Figure 15.46) [2].
- Orifice size. If an orifice is small, it is described as restrictive. It produces a high pressure gradient but a low flow rate, while a large shunt, which is described as non-restrictive, generates little or no gradient but a high flow rate. The shunt's direction is dependent on that of the pressure gradient. It may vary over the course of the cardiac cycle. The larger the shunt (i.e. the less restrictive it is), the more its flow rate is dependent on the ratio of pulmonary vascular resistance (PVR) to systemic vascular resistance (SVR). If the pressures equalise, the shunt becomes bidirectional. In this case, while O2 saturation in the pulmonary artery is higher than in the systemic venous return, saturation in the aorta is lower than in the pulmonary veins [4].
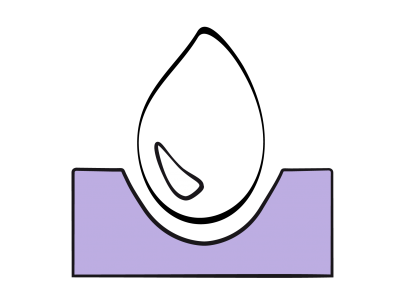
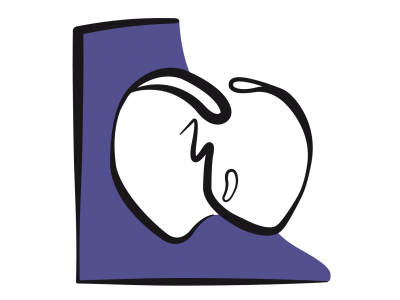
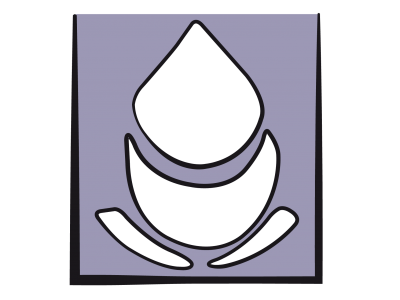
- Dilation of the receiving chambers. Shunts located upstream of the atrioventricular junction (ASD, anomalous pulmonary venous return) cause the right chambers to dilate, since the RV must pump the volume overload into the pulmonary artery. In contrast, if the shunt is located downstream of the atrioventricular junction (VSD, patent ductus arteriosus), the LV is the driving pump for the flow through the shunt. This flow mainly occurs during systole when the pulmonary valve is open. The RV operates as a passive conduit (Figure 15.6). In both cases, the pulmonary artery (PA) is dilated. Shunts located at ventricular and arterial level are dependent on the ratio of PVR to SVR, while shunts located at atrial level are more dependent on right and left ventricle compliance (diastolic dysfunction).
- Pulmonary blood flow. This may be increased (L-to-R shunt) or reduced (R-to-L shunt, pulmonary stenosis). A long-term increase in pulmonary blood flow can lead to pulmonary arterial hypertension (PAH) and RV pressure overload, while reduction of pulmonary blood flow leads to cyanosis.
Figure 15.6: Ventricular overload due to a L-to-R shunt. A: If the shunt is located upstream of the atrioventricular valves (ASD, anomalous pulmonary venous return), the RV is subjected to volume overload; the RA, RV and PA are dilated; tricuspid insufficiency (TI) is common. B: If the shunt is located downstream of the atrioventricular valves (VSD, patent ductus arteriosus), the LV is subjected to volume overload since the blood volume that it pumps returns to it after passing through the lungs; the PA, LA and LV are dilated; the RV only hypertrophies and dilates if pulmonary hypertension becomes established.
The value of a shunt (Qp/Qs) is the ratio of the pulmonary blood flow to the systemic blood flow. It can be calculated using echocardiography or catheterisation based on the ratio of the flow or stroke volume through the pulmonary artery and through the aorta (or the systemic outflow tract). A L-to-R shunt may be more reliably calculated by measuring oxygen enrichment in the pulmonary artery, i.e. based on the ratio between saturations (see Chapter 14, Shunts) [3]:
Qp / Qs = (SaO2 - SvO2) / (SpvO2 - SpaO2)
where: SaO2: arterial oxygen saturation
SvO2: central venous oxygen saturation (2 • SvO2 IVC + SvO2 SVC) / 3
SpvO2: oxygen saturation of the pulmonary veins
SpaO2: oxygen saturation of the pulmonary artery
and: SpvO2 ≈ SaO2 (mean of 96-98% at room air)
therefore: Qp / Qs = (SaO2 - SvO2) / (SaO2 - SpaO2)
In the example below, mixed venous blood (SvO2 74%) is enriched by a L-to-R shunt up to a value of 90% in the pulmonary artery:
(98% - 74%) / (98% - 90%)
Qp / Qs = 24 / 8 = 3:1
In this case, the ratio of pulmonary flow to systemic flow is 3:1.
| Shunts |
| A shunt has 4 characteristics: - Its direction (non-cyanotic L-to-R, cyanotic R-to-L) - Its size (restrictive or non-restrictive) - The dilation of the receiving chambers - The increase or decrease of pulmonary blood flow The shunt is defined by its ratio to systemic flow: Qp / Qs |
© BETTEX D, CHASSOT PG, January 2008, last update May 2018
References
- BETTEX D, CHASSOT PG. Transesophageal echocardiography in congenital heart disease. In: BISSONNETTE B, edit. Pediatric anesthesia. Basic principles, State of the art, Future. Shelton (CO): People’s Medical Publishing House (USA), 2011, 1186-1212
- CHASSOT PG, BETTEX DA. Anesthesia and adult congenital heart disease. J Cardiothorac Vasc Anesth 2006; 20:414-37
- DUPUIS C, KACHANER J, PAYOT M. Cardiologie pédiatrique (Paediatric cardiology) Paris: Flammarion, 1991, 137-42
- JOFFE DC, SHI MR, WELKER C. Understanding cardiac shunts. Ped Anaesth 2018; 28:316-25
- SILVERSIDES CK, DORE A, POIRIER N, et al. Canadian Cardiovascular Society 2009 Consensus Conference on the management of adults with congenital heart disease: Shunt lesions. Can J Cardiol 2010; 26:e70-e79
15. Anesthesia for adult congenital heart disease patients
- 15.1 Introduction
- 15.2 Nomenclature and pathophysiology
- 15.3 Approach by pathology
- 15.3.1 Classification
- 15.3.2 Diagnostic methods
- 15.3.3 Anomalous venous returns
- 15.3.4 Atrial septal defects (ASDs)
- 15.3.5 Atrioventricular canal (AVC) defects
- 15.3.6 Ebstein anomaly
- 15.3.7 Ventricular septal defects (VSDs)
- 15.3.8 Ventricular hypoplasia
- 15.3.9 Tetralogy of Fallot
- 15.3.10 Mixed shunt
- 15.3.11 Pulmonary stenosis
- 15.3.12 Anomalies of the LV ejection pathway
- 15.3.13 Transposition of the great arteries (TGA
- 15.3.15 Coarctation of the aorta
- 15.3.14 Congenitally corrected TGA
- 15.3.16 Arterial abnormalities
- 15.4 General considerations for anesthesia
- 15.5 Conclusions