Step 7 of 16
Ventricular septal defects (VSDs)
VSDs account for 10% of congenital heart disease encountered in adults and 30% of that detected at birth [2]. The interventricular septum is muscular, with the exception of its upper part situated below the aortic valve, which is membranous. Communication between the two ventricles may occur at four different locations (Figure 15.27) [1].

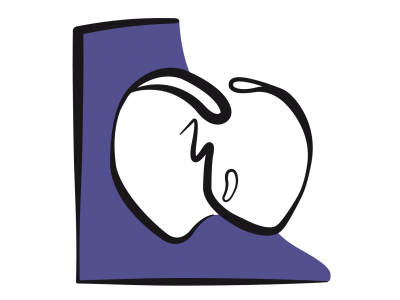
Figure 15.27: Diagram showing the various anatomical variants of ventricular septal defects (VSDs). VSDs of the membranous septum are typical of tetralogy of Fallot. Inlet VSDs are observed in AV canal defects. Basal VSDs (membranous septum, inlet and infundibular or supracristal) are located close to the RV outflow tract. Consequently, their flow bypasses the RV chamber (arrow) [5,6]. On the left is a diagram of the interventricular septum viewed from the RV.
Figure 15.27: Diagram showing the various anatomical variants of ventricular septal defects (VSDs). VSDs of the membranous septum are typical of tetralogy of Fallot. Inlet VSDs are observed in AV canal defects. Basal VSDs (membranous septum, inlet and infundibular or supracristal) are located close to the RV outflow tract. Consequently, their flow bypasses the RV chamber (arrow) [5,6]. On the left is a diagram of the interventricular septum viewed from the RV.
- Membranous or perimembranous VSD (Video and Figure 15.28): the most common type (70% of cases); typical of tetralogy of Fallot. It may gradually close spontaneously.
Video: Membranous VSD located under the aortic valve in a case of tetralogy of Fallot.
Figure 15.28: Membranous VSD. A: clearly visible orifice in the position where the membranous part of the interventricular septum should be located. Such VSDs are typical of tetralogy of Fallot. B : VSD in the process of closure by attachment of the septal leaflet of the tricuspid valve.
- Muscular VSD (20% of cases): often multiple (Swiss cheese septum), and may close by hypertrophy of the septum (Video and Figure 15.29) .
Video: muscular VSD through the interventricular septum; the colour flow shows the L-to-R crossing.
Figure 15.29: TEE image of a muscular VSD. Although it normally meanders between the trabeculations and is only clearly visible with colour flow (left), the VSD shown on the right is a neat perforation, which is relatively rare.
- Inlet VSD (5-10% of cases): part of AV canal defects, appearing below and between the septal leaflets of the mitral valve and tricuspid valve (Video and Figure 15.30); it may be spontaneously occluded by the tricuspid valve's septal leaflet.
Video: Inlet VSD located under the tricuspid valve in a case of AV canal.
Figure 15.30: TEE images of an inlet VSD located below the tricuspid valve in the proximal part of the interventricular septum. This type of VSD is part of the AV canal defect, which in this case is partial as there is no associated ostium primum ASD. The septal insertions of the mitral and tricuspid valve are at the same level, which is typical of an AV canal defect.
- Infundibular or supracristal VSD (5% of cases) (Video and Figure 15.31): located just below the pulmonary valve, it communicates with the left outflow tract below the aortic valve. This proximity frequently causes one or two cusps of the aortic valve to prolapse (right coronary and, more rarely, non-coronary cusps), resulting in aortic insufficiency.
Video: Infundibular VSD, located under the aortic valve; the communication is between the left and right outflow tracts; presence of a small aortic regurgitation.
Figure 15.31: Image of an infundibular or supracristal VSD located below the aortic valve. The crossing is revealed by the colour Doppler flow. This VSD causes the two outflow tracts to communicate with each other. LVOT: left ventricular outflow tract. RVOT: right ventricular outflow tract.
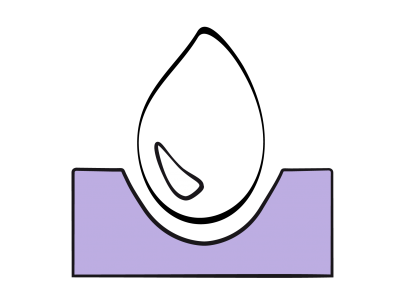
Spontaneous closure is quite a common event for inlet VSDs, perimembranous VSDs and muscular VSDs, occurring in 40% of cases [13]. The VSD produces a non-cyanotic L-to-R shunt that overloads the pulmonary circulation. Contrary to acquired VSDs, which are muscular, inferior and apical, most congenital VSDs are anatomically located very high at the level of the ventricular inlet and outflow tract. Blood following the shunt in a sense bypasses the right ventricular chamber. The LV performs the necessary work in terms of pressure and volume, acting as the driving force pumping the blood through the shunt and lungs. The RV is a passive, non-contributive conduit and only hypertrophies if pulmonary hypertension develops. The VSD therefore causes volume overload for the LV, which must pump the blood through the shunt into the pulmonary circulation. This volume is returned to it via the LA (Video and Figure 15.32). Therefore, the first issue facing patients with a VSD is left-sided failure (Figure 15.33) [4].
Video: Dilatative hypertrophy of the left ventricle due to the volume overload in a case of VSD.
Figure 15.32: Diagram showing shunting caused by a VSD. Blood pumped by the LV through the VSD is ejected into the PA and then returned to the LA and LV. Volume overload therefore occurs in the left ventricle. The right ventricle functions as a passive conduit and only hypertrophies if pulmonary pressure is high.
Figure 15.33: LV volume overload and dilation in a VSD case.
Auscultation reveals a rasping, irradiant, murmur radiating in all directions from the left border of the sternum with a pronounced systolic thrill. Adult patients may be subdivided into four groups based on the lesion’s haemodynamic impact [8,12,19].
- Spontaneously or surgically closed VSD – there is no longer any shunting or merely a minimal residual flow without any haemodynamic significance. Right-sided pressure is normal. The life expectancy of these patients is normal if closure occurs before the age of 3 years.
- Small, restrictive VSD with limited shunting – pulmonary blood flow is slightly increased and pulmonary pressure is at the upper limit of normal levels, but no PAH develops. Even though the risk of endocarditis is increased, life expectancy is good.
- Moderate VSD with significant shunting – pulmonary pressure is high. The RV is hypertrophied. Life expectancy is 86% at 25 years.
- Non-restrictive VSD and severe PAH with Eisenmenger's syndrome (PVR > 800•dynes•cm s-5) and bidirectional shunting (see Pulmonary hypertension). Pressure overload causes hypertrophy followed by right ventricular failure with dilation of the RV, tricuspid insufficiency, and systemic stasis. The shunt’s flow rate decreases due to the gradual equalisation of pressure between the LV and RV. Without treatment, 40% of patients die before the age of 25 years. Surgical correction is contraindicated if the PVR/SVR ratio is > 0.7 as the risk is prohibitive [7].
On echocardiographic examination, the pulmonary artery and left chambers are dilated as they are the shunt's receiving chambers [3,5,10]. The RV becomes hypertrophied and dilated in proportion to the degree of pulmonary hypertension. Doppler echocardiography reveals the L-to-R crossing flow. This exhibits several characteristics (Figure 15.34).

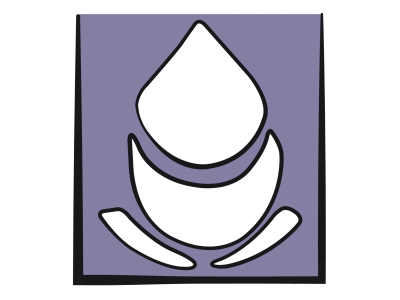
Figure 15.34: Characteristics of VSD flow. With colour Doppler, a proximal isovelocity surface area (PISA) is visible upstream of the orifice, on the left ventricular side; the swirls appear inside the RV chamber. The flow can be tracked through the VSD. On a spectral Doppler, the image shows a systolic-diastolic flow that is predominantly systolic. The flow velocity is dependent on the pressure gradient between the RV and LV. It decreases as pulmonary hypertension and right heart decompensation become established. Diastolic flow may invert (R-to-L) in the event of right heart failure, with EDP rising higher on the right side than on the left. The dotted line shows a muscular VSD flow, with the conduit temporarily obstructed by myocardial contraction during systole.
Figure 15.34: Characteristics of VSD flow. With colour Doppler, a proximal isovelocity surface area (PISA) is visible upstream of the orifice, on the left ventricular side; the swirls appear inside the RV chamber. The flow can be tracked through the VSD. On a spectral Doppler, the image shows a systolic-diastolic flow that is predominantly systolic. The flow velocity is dependent on the pressure gradient between the RV and LV. It decreases as pulmonary hypertension and right heart decompensation become established. Diastolic flow may invert (R-to-L) in the event of right heart failure, with EDP rising higher on the right side than on the left. The dotted line shows a muscular VSD flow, with the conduit temporarily obstructed by myocardial contraction during systole.
- Systolic and diastolic flow – the systolic component exhibits a maximum velocity of 2-4 m/s. It is reduced or absent in muscular VSDs due to contraction of the myocardium.
- In restrictive shunts (small orifice), the flow’s Vmax is high (4 m/s) and strictly L-to-R in direction. In non-restrictive shunts (large orifice), left and right pressure tends to equalise and the flow's Vmax is low. These shunts may become bidirectional.
- Continuous crossing on colour flow with receiving swirls in the RV, which are generally more clearly visible during diastole as they are carried away by the normal flow in systole.
- Concentric acceleration zone (PISA: proximal isovelocity surface area) – if the shunt is restrictive, the size of the PISA is proportional to the quantity of blood passing through the VSD (Vidéo CIV flux) [11]. The PISA is absent in non-restrictive shunts.
If a VSD is present, the prevailing pressure in the RV during systole is contaminated by that of the LV, which pumps the shunt flow. This skews the calculation of pulmonary pressure using TI velocity (see Figure 15.7). However, it is possible to calculate RV systolic pressure based on the shunt flow velocity. The maximum shunt velocity (Vmax) represents the pressure difference between the LV and RV during systole. When subtracted from systemic arterial pressure (APs) (assuming no aortic pathology), it gives RV systolic pressure (Ps) [5]:
RVPs = APs - 4 (Vmax VSD)2
Surgical closure of the VSD (patch or direct closure) is imperative if the shunt is moderate or major (Qp/Qs ≥ 1.5) if: the LV is dilated due to volume overload; the lesion is part of a complex anatomical syndrome (AV canal defect, tetralogy of Fallot); or it is located between the outflow tracts due to the risk of aortic insufficiency [9,15,16]. A correction performed in the first three years of life will preserve ventricular function and normal pulmonary circulation. However, due to the proximity of conduction bundles, bundle branch blocks or complete AV blocks are common postoperatively and a high proportion of patients are dependent on a permanent pacemaker [14]. Many muscular VSDs and some perimembranous VSDs can be occluded percutaneously with a very low morbidity and mortality rate (1-2%). The most common complications post-correction are: aortic or tricuspid insufficiency, residual VSD, obstruction of an outflow tract, and AV blocks. Closure of the VSD is contraindicated if the PVR/SVR ratio is > 0.65, mPAP > 0.5 mAP, or in the event of irreversible PAH [15,16,18].
Anaesthesia
In order to avoid destabilising haemodynamics, attempts are made to ensure conditions that decrease the flow rate of L-to-R shunting (see Figure 15.20). These are:
- Reduced systemic pressure (arterial vasodilation);
- Increased right-sided pressure (pulmonary vasoconstriction).
General anaesthesia is conducted under slight hypercapnia, low FiO2 (0.3) and PEEP, with an agent such as isoflurane. This approach is valid unless there is pre-existing pulmonary hypertension, in which case this pathology takes priority. In non-cardiac surgery, neuraxial blockade fully meets the required conditions [6].
Patients with VSDs are highly sensitive to hypovolaemia. Although their circulating volume is increased, some of this volume is simply circulating through the lungs due to the shunt. This portion is unavoidable: it is dependent on the orifice diameter and is subjected to pressure levels that are lower than systemic pressure. A loss of circulating volume therefore occurs mainly at the expense of peripherally circulating volume. Arterial vasoconstriction due to hypovolaemia merely prompts a greater proportion of volume to flow into the shunt’s circuit at the expense of systemic perfusion. Furthermore, VSD is the heart disease causing the fewest arrhythmias [2].
Following VSD correction by patch, a small residual leak is tolerable provided that the following conditions are met [17]:
Patients with VSDs are highly sensitive to hypovolaemia. Although their circulating volume is increased, some of this volume is simply circulating through the lungs due to the shunt. This portion is unavoidable: it is dependent on the orifice diameter and is subjected to pressure levels that are lower than systemic pressure. A loss of circulating volume therefore occurs mainly at the expense of peripherally circulating volume. Arterial vasoconstriction due to hypovolaemia merely prompts a greater proportion of volume to flow into the shunt’s circuit at the expense of systemic perfusion. Furthermore, VSD is the heart disease causing the fewest arrhythmias [2].
Following VSD correction by patch, a small residual leak is tolerable provided that the following conditions are met [17]:
- Residual VSD diameter < 2 mm;
- No flow convergence area on the left side;
- Enrichment of saturation in the PA < 5%.
A thorough examination of the tricuspid valve is recommended, since the septal leaflet may undergo tethering on closure of a perimembranous or inlet VSD. During repairs of infundibular VSDs, the right coronary cusp or non-coronary cusp of the aortic valve may be retracted, resulting in aortic insufficiency. The right transatrial repair technique requires partial detachment of the tricuspid valve, which must then be reconstructed. The degree of residual leakage must be clearly assessed [4].
© BETTEX D, CHASSOT PG, January 2008, last update February 2020
References
| Ventricular septal defects (VSDs) |
| Characteristics: - Non-cyanotic L → R shunt, increased pulmonary blood flow (Qp ↑, Qp/Qs > 1.5) - Dilated receiving chambers: PA, LA, LV - Volume overload for the LV - Restrictive shunt: PAP at the upper limit of normal levels - Non-restrictive shunt: PAH, pressure overload for the RV, RVH - Severe PAH in 50% of adults (PVR 500-800 dynes•cm•s-5) To reduce the shunt: reduce SVR, increase PVR (if PAH is absent) Anaesthesia recommendations: - GA with isoflurane - Neuraxial blockade (spinal anaesthesia, epidural) - Ventilation: FiO2 0.3, hypercapnia (unless PAH) - Hypovolaemia poorly tolerated due to sequestration of volume in the pulmonary circuit - Where appropriate, specific management of LV failure and PAH (RVH) |
© BETTEX D, CHASSOT PG, January 2008, last update February 2020
References
- AMMASH NM, WARNES CA. Ventricular septal defects in adults. Ann Int Med 2001; 135:812-9
- BAUMGARTNER H, BONHOEFFER P, DE GROOT NMS, et al. ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J 2010; 31:2915-57
- BETTEX D, CHASSOT PG. Malformations congénitales de l'adulte. In: BETTEX D, CHASSOT PG. Echocardiographie transoesophagienne en anesthésie – réanimation. Paris: Pradel-Masson, Williams & Wilkins, 1997, 171-87
- BHATT AB, FOSTER E, KUEHL K, et al. Congenital hesart disease in older adult. A Scientific Statement from the American Heart Association. Circulation 2015; 131:1884-931
- CHASSOT PG, BETTEX D. Perioperative transoesophageal echocardiography in adult congenital heart disease. In: POELAERT J, SKARVAN K. Transoesophageal echocardiography in anaesthesia. London, BMJ Book, 2004
- CHASSOT PG, BETTEX DA. Anesthesia and adult congenital heart disease. J Cardiothorac Vasc Anesth 2006; 20:414-37
- DALIENTO L, SOMERVILLE J, PRESBITERO P, et al. Eisenmenger syndrome. Factors relating to deterioration and death. Eur Heart J 1998; 19:1845-55
- KIDD L, DRISCOLL DJ, GERSONY WM, et al. Second natural history study of congenital heart defects. Results of patients with ventricular septal defects. Circulation 1993; 87(Suppl I):38-51
- LUN K, LI H, LEUNG MP. Analysis of indications for surgical closure of subarterial ventricular septal defect without aortic cusp prolapse and aortic regurgitation. Am J Cardiol 2001; 87:1266-70
- MILLER-HANCE WC, SILVERMAN NH. Transesophageal echocardiography (TEE) in congenital heart disease with focus on the adult. Cardiol Clinics 2000; 18:861-92
- MOISES VA, MACIEL BC, HOMBERGER LK, et al. A new method for non-invasive estimation of ventricular septal defect shunt flow by color Doppler flow mapping: imaging of the laminar flow convergence region on the left septal surface. J Am Coll Cardiol 1991; 18:824-32
- NEUMAYER U, STONE S, SOMERVILLE J. Small ventricular septal defects in adults. Eur Heart J 1998; 19:1573-82
- PERLOFF JK. Survival patterns without cardiac surgery or interventional catheterization: a narrowing base. In: PERLOFF JK, CHILD JS, Eds. Congenital heart disease in adults. 2nd edition. Philadelphia: WB Saunders, 1998, 15-53
- PERLOFF JK, WARNES CA: Challenges posed by adults with repaired congenital heart disease. Circulation 2001; 103:2637-43
- SILVERSIDES CK, DORE A, POIRIER N, et al. Canadian Cardiovascular Society 2009 Consensus Conference on the management of adults with congenital heart disease: Shunt lesions. Can J Cardiol 2010; 26:e70-e79
- STOUT KK, DANIELS CJ, VALENTE AM, et al. 2018 AHA/ACC Guideline for the management of adults with congenital heart disease. J Am Coll Cardiol 2019; 73:e81-192
- TEE SDG, SHIOTA T, WEINTRAUB R, et al. Evaluation of ventricular septal defect by transesophageal echocardiography: Intraoperative assessment. Am Heart J 1994; 127:585-92
- WARNES CA, WILLIAMS RG, BASHORE TM, et al. ACC/AHA 2008 Guidelines for the management of adults with congenital heart disease: executive summary. Circulation 2008; 118:2395-451
- WEIDMAN WH, DUSHANE JW, ELLISON RC. Clinical course of adults with ventricular septal defect. Circulation 1977; 56(Suppl I):78-9
15. Anesthesia for adult congenital heart disease patients
- 15.1 Introduction
- 15.2 Nomenclature and pathophysiology
- 15.3 Approach by pathology
- 15.3.1 Classification
- 15.3.2 Diagnostic methods
- 15.3.3 Anomalous venous returns
- 15.3.4 Atrial septal defects (ASDs)
- 15.3.5 Atrioventricular canal (AVC) defects
- 15.3.6 Ebstein anomaly
- 15.3.7 Ventricular septal defects (VSDs)
- 15.3.8 Ventricular hypoplasia
- 15.3.9 Tetralogy of Fallot
- 15.3.10 Mixed shunt
- 15.3.11 Pulmonary stenosis
- 15.3.12 Anomalies of the LV ejection pathway
- 15.3.13 Transposition of the great arteries (TGA
- 15.3.15 Coarctation of the aorta
- 15.3.14 Congenitally corrected TGA
- 15.3.16 Arterial abnormalities
- 15.4 General considerations for anesthesia
- 15.5 Conclusions